As someone who has had PCOS, I know firsthand how overwhelming the condition can be. The irregular periods, the hormonal fluctuations, the struggles with energy and mood. PCOS can feel all-encompassing. But one of the most empowering steps I’ve taken is understanding how this condition works on a physiological level. By knowing what’s happening inside my body, I’ve been able to tailor my lifestyle and nutrition to regain balance. In this post, I’ll break down the science behind PCOS and how holistic habits like managing blood sugar, eating whole foods, and staying active can make all the difference.
The physiology of PCOS: understanding androgen production
PCOS is a hormonal disorder, and it involves more than just your reproductive system. It’s a condition that affects how your body processes and produces certain hormones, particularly androgens (like testosterone). Androgens are considered “male hormones,” but they play important roles in women’s bodies, too — just in smaller amounts. In women with PCOS, androgen levels are often higher than normal, which leads to many of the symptoms we experience, from acne to irregular periods.
Androgens are produced in the ovaries, adrenal glands and in fat tissue.
- Ovaries: Your ovaries produce about 25% of your testosterone and 50% of androstenedione, a precursor to testosterone. They also contribute a smaller amount of DHEA (about 20%).
- Adrenal glands: These glands are also significant players, contributing about 25% of your testosterone and the bulk of DHEA (around 80%). The adrenal glands also produce DHEA-S, which can be a marker of adrenal-driven PCOS.
- Fat tissue: Interestingly, fat tissue plays a role in androgen production, too, converting androstenedione into testosterone. This is why maintaining a healthy weight can be so important for managing PCOS.
Testing is SO important to understand whether the source of elevated androgens in your body is from your ovaries or adrenal glands. If you have elevated DHEA-S, for example, your excess androgens may be adrenal-driven. High levels of testosterone, on the other hand, could point to ovarian sources. Knowing this distinction helps personalize treatment, which is why I always advocate for a thorough hormonal panel.
Insulin resistance: the silent driver behind PCOS
One of the lesser-known but extremely important factors in PCOS is insulin resistance. Insulin is a hormone that helps your body use glucose (sugar) from the food you eat for energy. When you have insulin resistance, your cells don’t respond well to insulin, which causes your pancreas to produce more insulin to compensate. This excess insulin can stimulate the ovaries to produce even more androgens, exacerbating PCOS symptoms.
Because of this, managing insulin and blood sugar levels is essential to controlling PCOS. This is where nutrition and lifestyle habits become critical.
Nutrition: managing blood sugar with whole foods
In my experience, one of the most effective ways to manage PCOS is through blood sugar control. A huge part of this involves eating whole, balanced meals three times a day. I focus on meals that include a combination of:
- Protein: These help stabilize blood sugar and reduce cravings.
- Healthy fats: Fats like avocado, olive oil, and butter are important for hormone production and keeping you full longer.
- Fiber-rich carbs: Whole grains, legumes, and vegetables help keep blood sugar stable.
By minimizing sugar and processed foods, you reduce insulin spikes, which in turn helps lower androgen production. For those of us with PCOS, this isn’t just about avoiding weight gain — it’s about balancing hormones and reducing inflammation.
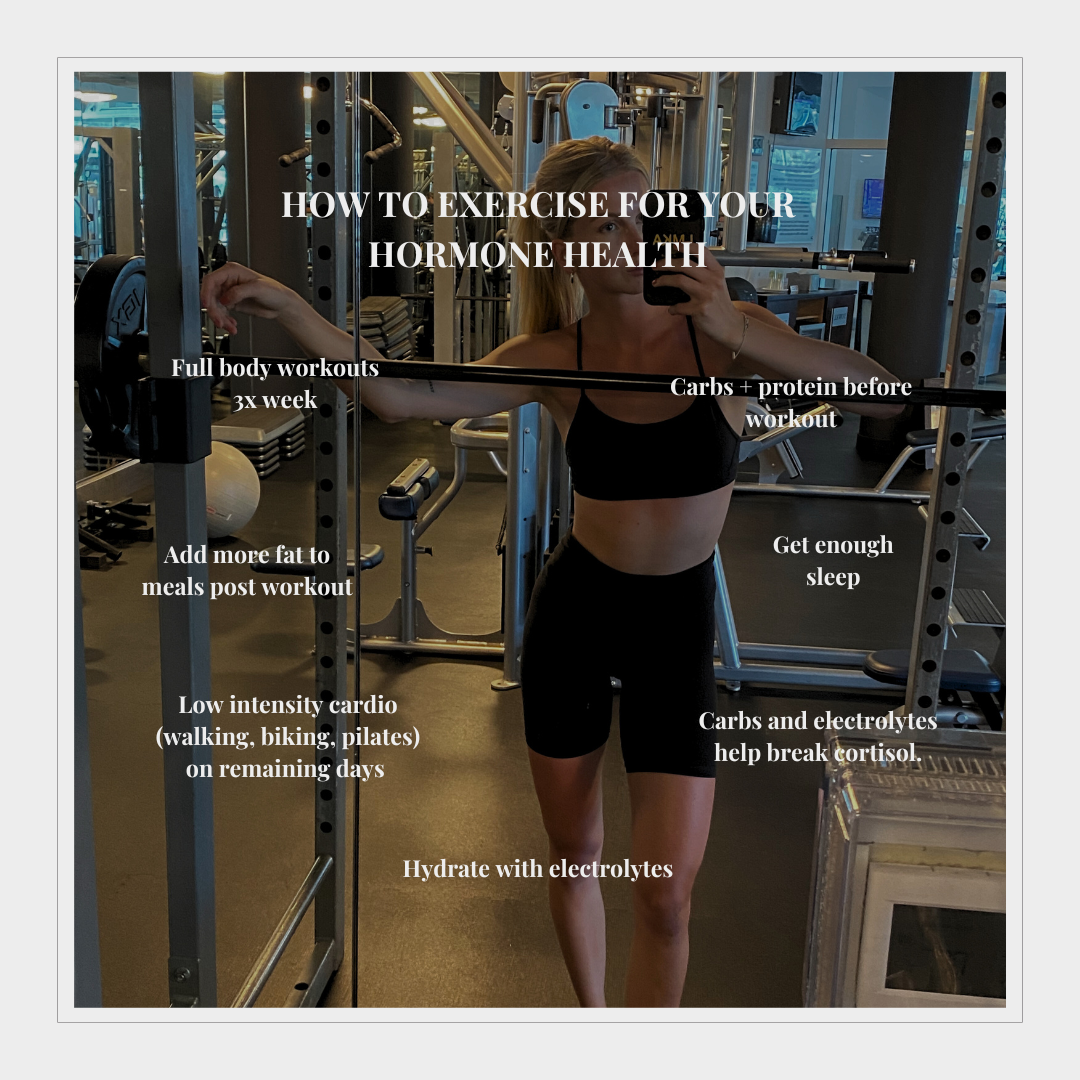
Exercise: resistance training and walking for hormonal balance
While nutrition lays the foundation, movement is the other half of the equation. Resistance training is one of the most effective forms of exercise for PCOS because it builds muscle, which improves insulin sensitivity. The more muscle you have, the better your body becomes at using glucose, which helps regulate blood sugar and prevent insulin resistance from getting worse.
I also make it a point to walk daily, even if it’s just for 20 to 30 minutes. Walking helps lower cortisol (the stress hormone), improves blood sugar regulation, and keeps you in a healthy rhythm. If you’re new to exercise or feel overwhelmed by starting a routine, simply adding a walk after meals can have a big impact.
Stress management: controlling cortisol and supporting adrenal health
Stress is another major factor in PCOS, especially for those of us with adrenal-driven PCOS. Elevated cortisol from stress can lead to more androgen production, making symptoms worse. That’s why managing stress is essential for hormonal balance. Practices like meditation, deep breathing, and spending time outdoors are all good methods to reduce cortisol levels.
My experience with post-pill PCOS
After stopping birth control, I experienced the sudden onset of post-pill PCOS. The hormone fluctuations after coming off the pill can trigger PCOS symptoms, and I found myself dealing with acne, irregular periods, and fatigue. It took time, but with a combination of whole-foods nutrition, regular exercise, and stress management, I was able to restore balance in my body.
If you’re navigating post-pill PCOS, know that it’s possible to regain your hormonal balance with consistent healthy habits. Don’t be discouraged if it takes time — I t’s a marathon, not a sprint.
How to check if you have PCOS
If you suspect you might have PCOS, it’s important to get a proper diagnosis. PCOS is often diagnosed based on a combination of symptoms, hormone levels, and sometimes imaging. Here are the key symptoms to watch for:
- Irregular periods or no periods at all
- Excess androgen symptoms like acne, excess facial or body hair (hirsutism), or thinning hair on the scalp
- Weight gain or difficulty losing weight
- Ovarian cysts (though not always present)
- Fatigue or trouble sleeping
- Mood changes like anxiety or depression
- Insulin resistance or blood sugar issues, sometimes leading to cravings or crashes after meals
Testing for PCOS
If you’re experiencing these symptoms, working with a functional practitioner or gynecologist is essential for getting the right tests and a clear diagnosis. Here are some common tests that can help identify PCOS:
- Blood tests to check hormone levels, particularly testosterone, DHEA, LH, FSH, and insulin.
- Ultrasound to look for ovarian cysts, though not all women with PCOS have cysts.
- DUTCH test (Dried Urine Test for Comprehensive Hormones): This is a highly detailed test that can give insight into both your adrenal and ovarian hormone levels, including cortisol patterns and androgen metabolites. It’s a great option for understanding more about your hormone health.
- Thyroid panel to rule out conditions like hypothyroidism, which can mimic some PCOS symptoms.
- Blood sugar and insulin testing to check for insulin resistance.
Seek professional guidance
If you’re experiencing any of these symptoms or suspect PCOS, don’t hesitate to seek help from a healthcare professional. A functional medicine practitioner, gynecologist, or endocrinologist can help guide you through the right tests and create a personalized treatment plan that addresses your specific needs.
Managing PCOS doesn’t have to be complicated. Start by focusing on eating balanced meals, resistance training and daily walks, and managing stress. Each small step adds up.
Leave a Reply